Parenting young children is challenging enough under usual circumstances. But as we know, the past year has been anything but usual. As the community got vaccinated and resumed in-person learning in schools and early education settings, surges of COVID-19 infections meant that programs and families often had to pivot back to virtual services, often with short notice.
One such program is Dimock’s Early Intervention (EI) Program. EI provides children from birth to age three with critical services to help them reach their developmental milestones. Dimock’s program typically provides both home-and community-based support and activities based in our Jackie Jenkins-Scott Building.
This ability of Dimock’s EI program to transition back and forth seamlessly between in-person and online programming allows for the continuity of care that families need now more than ever.
“Throughout the COVID-19 pandemic, we’ve needed to pivot our in-home and center-based service model to allow for physical distancing,” says Jessica Nuhibian, Director of Dimock’s EI program. She is careful not to use the term ‘social distancing’ because social connection is vital for young children and their families— and is still possible to sustain even during a pandemic.
For Dimock providers, it was essential to maintain the continuity of care that their families had come to rely on during this challenging time and provide ongoing opportunities for children to learn and grow. “Our team has been so wonderful and fluid in finding creative ways to make sure families can stay connected and still access services even when so much changes from day to day,” Jessica explains.
In some ways, virtual learning can be even better than in-person learning. “Seeing facial movement and expression is an essential part of supporting early social-emotional and communication development, and that is not possible right now while wearing a mask,” says Jessica. “So, in a number of ways, having continued access to telehealth has allowed us to better serve our families.”
One important—and fun—way that families were able to interact safely is through an expressive therapy playgroup which uses music and movement to provide opportunities for connection and learning. Casara Nemes, the group facilitator, explains, “Children have the opportunity to learn social skills that will benefit them when they return to in-person interactions—such as turn-taking, show and tell, and using communication to share their wants.”
Since the pandemic began, this playgroup has been adapted for the virtual space. And it’s been a hit with children and their caregivers alike.
“We’ve been isolated for so much of the COVID-19 pandemic, so participating in the virtual playgroups helps us to feel engaged in the community,” shares Carmen, who attends the expressive therapy playgroups with her daughter Luna and husband José.

Luna was referred for a speech and motor skill delay at her first birthday, but she was at risk for other delays, as well. She was born with a congenital heart condition that required surgery when she was an infant. The surgery meant that she couldn’t spend time on her belly at the stage when babies would typically be practicing tummy time and learning to crawl.
Her EI Service Coordinator got to know Luna and helped her family connect with a variety of other services, including support around feeding and sleep. They also worked with Carmen and José to find strategies to help Luna crawl, communicate, walk, and interact with other children. Luna even took her first steps on Dimock’s campus, an experience her mom says she’ll never forget. Carmen shares about her Dimock EI team, “They go above and beyond and helped us with the whole picture of parenthood, not just with the therapies. They celebrate all the victories with us.”
Since Luna’s graduation from the program, the family has opted to stay involved and help other families get the most out of their EI experience. They now continue to participate in the virtual playgroups as “Community Peers,” modeling for other families how they incorporate the strategies they’ve learned in EI into their daily routines, and helping them feel comfortable being silly and playful with their children.
Sometimes it’s just important for caregivers to have someone to talk to and hear that they are doing all right, especially if they just received the news that their child is facing a developmental delay or have received a new diagnosis. “Our EI program continues to promote kids’ healthy development and support caregivers as they navigate complex systems. We do it in whatever way we can— whether that’s in person, on Zoom, or on the phone,” Jessica proudly shares. “We’re here to partner with families as members of their child’s team and to let them know that we are in this together.”





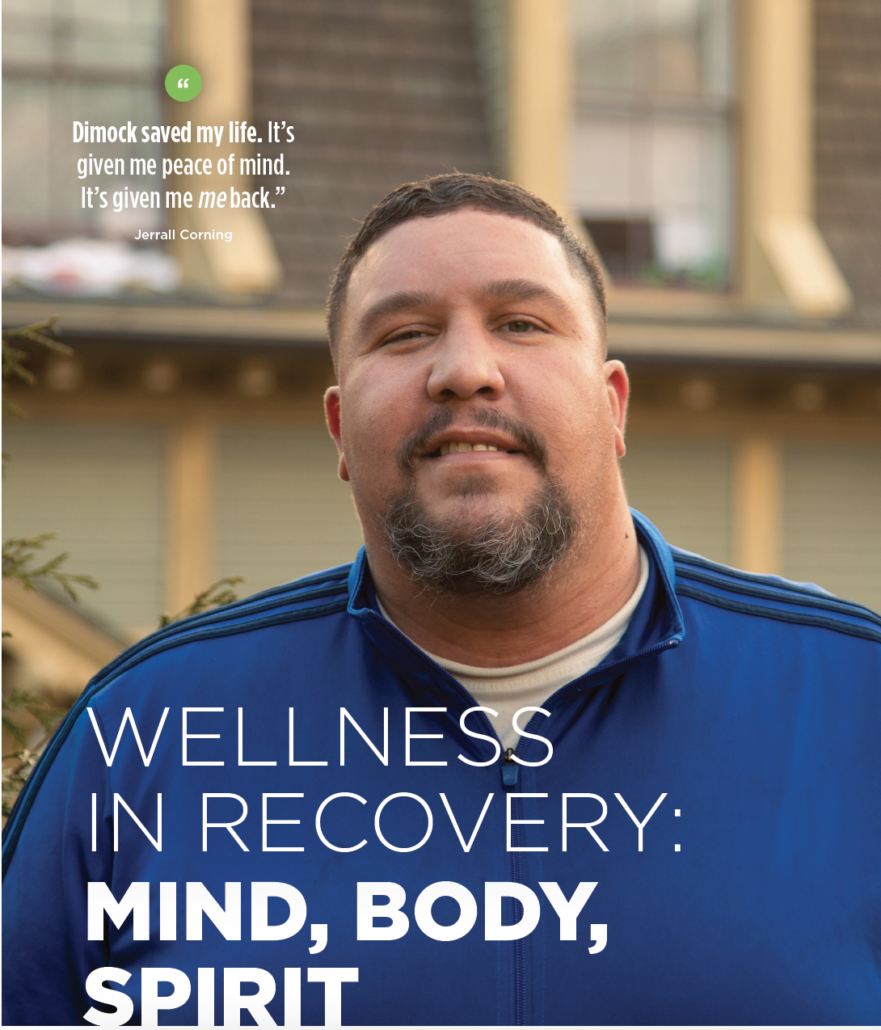
 “What first brought me to Dimock was all the resources that they have for us,” says Lissette Santos, a resident of My Sister’s House. “I go to therapy here and I participate in the fitness program every Tuesday and Thursday. I’m also doing anger management and relapse prevention programs here. The staff here stand by me and never let me down.”
“What first brought me to Dimock was all the resources that they have for us,” says Lissette Santos, a resident of My Sister’s House. “I go to therapy here and I participate in the fitness program every Tuesday and Thursday. I’m also doing anger management and relapse prevention programs here. The staff here stand by me and never let me down.”